Based on the eight findings discussed here, RHI has created a Blueprint laying out the full range of healthcare services that are clinically effective and financially sustainable across all of rural North Carolina.
The Blueprint
Customized for each of the state’s 22 rural regions, the Blueprint seeks to match healthcare resources to population needs based on three factors:
- Proximity – the right services have to be available at the right distance
- Complexity – from routine to specialized, we have to provide the fullest range of services that is sustainable for each region
- Stability – we have to reduce duplicative, undifferentiated services so that financially stable providers are able to invest in the services that communities actually need
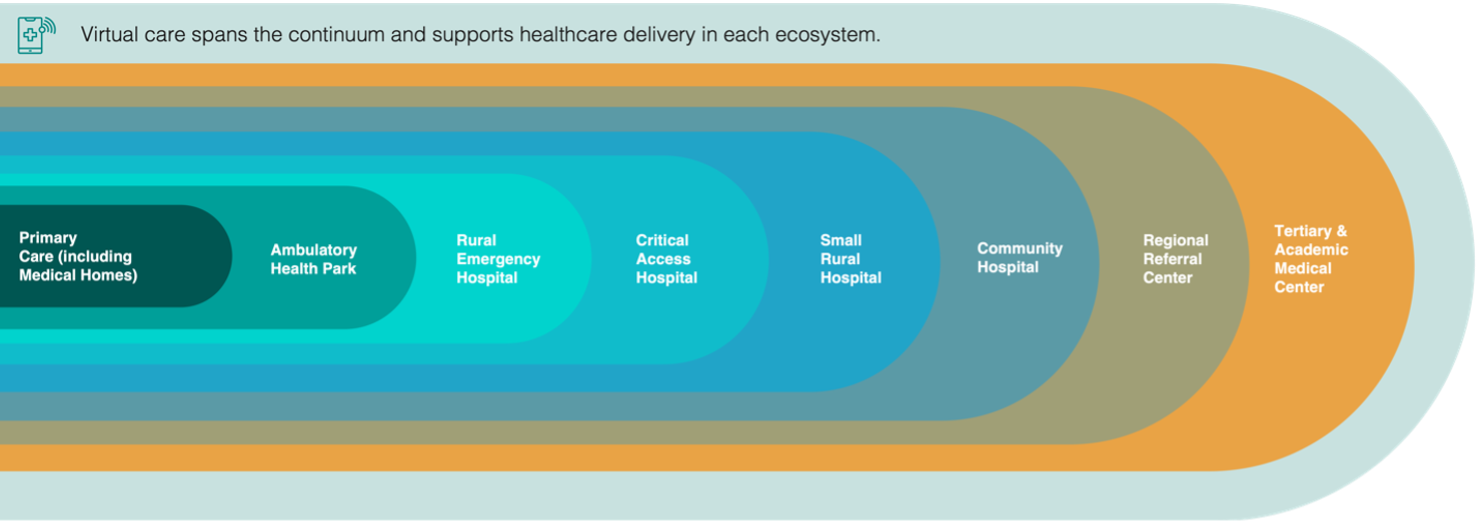
In each region, we identify eight access points for various healthcare needs, ranging from individual physician practices all the way through academic medical centers. Though no AMCs are located within a rural county, they are relevant to our analysis due to their anchor role in healthcare delivery statewide. Specific services can be delivered in multiple settings. For instance, chemotherapy can be offered to cancer patients at ambulatory health parks, not just hospital facilities.
Rather than fixed and immoveable features of the landscape, we treat these access points as “levers” that can be adjusted to achieve the goals of proximity, complexity, and stability. Many regions have too many hospital beds for treating low-acuity patients but too few providers in primary and specialty care. That creates poor health outcomes for individuals who don’t get the preventive care they need and poor financial performance for hospitals with expensive beds they can’t fill.
Creating a Sustainability Score
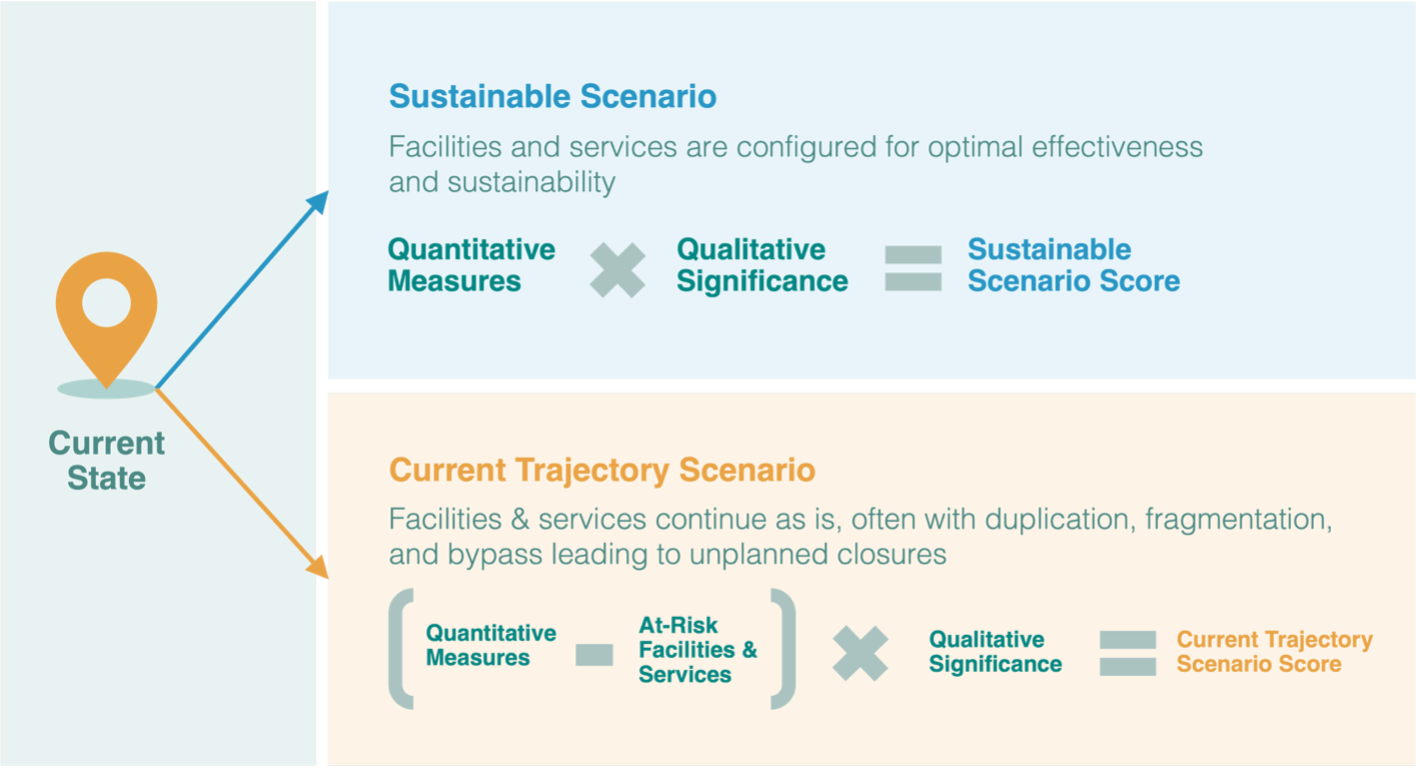
For each region, we created a three-part score indicating the status quo and two future scenarios. Potential scores ranged from 0 to 100.
- The current state score shows how well healthcare resources are matched to community needs based on objective measures used throughout this report – for instance, what percentage of the population lives within 60 minutes of a regional referral center or within 30 minutes of an ED.
- Next, we created a current trajectory scenario score – that is, what will likely happen to a region’s healthcare if no intentional steps are taken to improve sustainability. The major risk factor in this score is the unplanned closure of a hospital, with all of the service losses and clinician exits that follow. A lower trajectory score indicates that at least some hospitals in that region are at greater risk.
- Finally, we created a sustainable scenario score that indicates how regional healthcare could improve with the implementation of this Blueprint. A higher sustainability score means that residents have better access to the services they need most, and those services are financially sustainable under market conditions. The sustainability score does not mean that every hospital continues to operate in its current form. We recognize that change is inevitable, but planned, orderly change can be an opportunity for improvement.
Regarding the current trajectory, it is important to note that we calculated closure risk based on current payment realities, including Medicaid expansion and HASP payments. These recent payment policies have provided a lifeline to many rural hospitals, putting them on much firmer financial footing. If those reimbursements were cut due to policy changes in Washington or Raleigh, the risk score would change dramatically for the worse. In other words, our risk score is the best-case scenario. We have not attempted to quantify a worst-case scenario with the removal of Medicaid or HASP funding, but we would anticipate uncontrolled rural hospital closures across the state, creating further delays and hardships for residents forced to seek care far from home.
This three-sided scoring allows us to measure the urgency – or potential – of applying the Blueprint. In some regions, things are functioning well as is, and very little change is needed. In other regions, healthcare services and needs are severely mismatched, indicating the greatest need for improvement.
Applying the Blueprint
Finding a sustainable balance is central to the Blueprint, and that looks different in every rural region. Shifting resources may require difficult choices in some cases, but it also opens countless new possibilities, such as new regional referral centers caring for complex patients closer to home.
We detailed data and optimized resource mapping for all 22 regions covering 78 rural counties. Here we offer a hypothetical case study based on synthesized data from multiple regions. We’ll call this Sample Region Z.
Region Z comprises four counties with a combined population of 200,000. The region skews older, with many lower-income retirees who need regular medical care for multiple chronic conditions. Three hospitals currently serve the region. None has more than 65 beds, none has the resources to offer specialized services such as cardiac catheterization, and one – classified as a small rural hospital – is on the brink of closure due to consistently poor financial performance. Primary care offices are clustered close to the hospital campuses, so many residents drive 45 minutes or more to see their provider. All emergency services are located on hospital campuses, leaving one entire county with no convenient ED access. Combining all of these factors and more yields a current score of 53.0 for hypothetical Region Z.
The status quo is hardly ideal, but even that is not sustainable. Without some form of government intervention or investment, the small rural hospital is virtually certain to close. Many affiliated providers will be forced to relocate their practice, and one ED will be lost. This reduction in services and increase in drive times yields a score of 45.0 – a clear warning sign of deteriorating healthcare access for the rural population of these four counties.
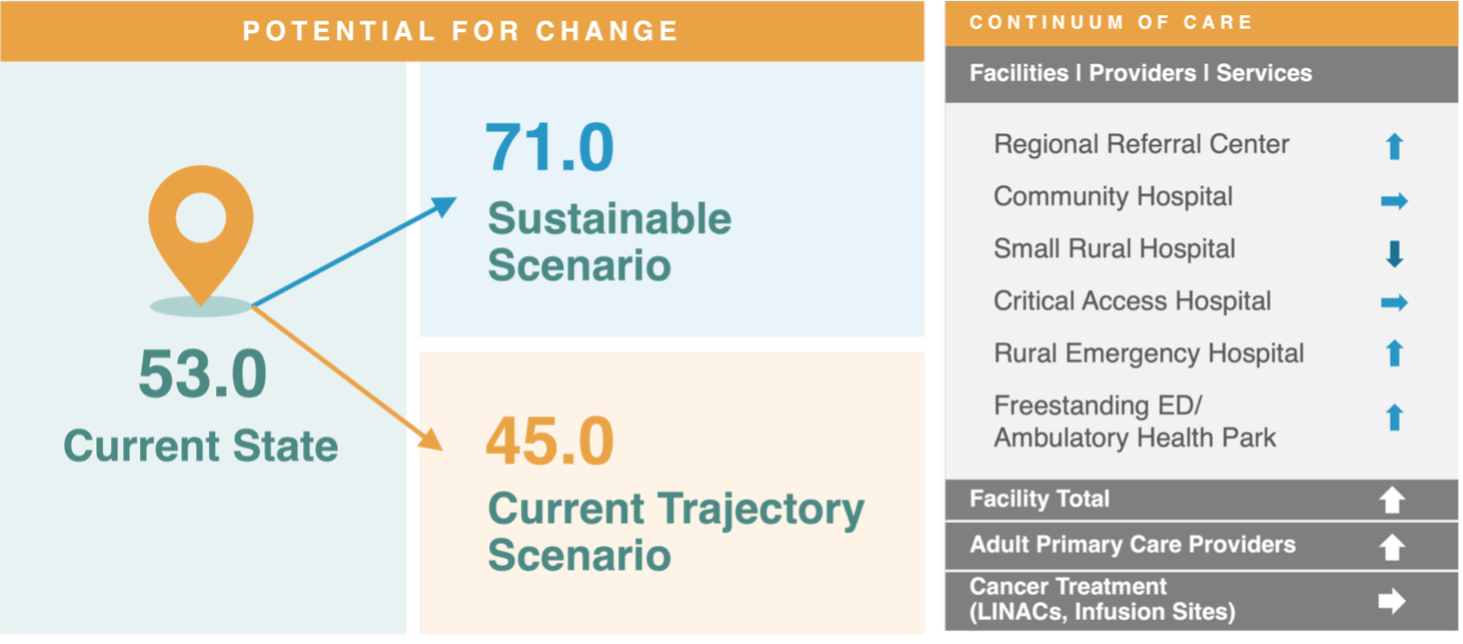
The Blueprint for Region Z recognizes that the small rural hospital is draining scarce resources that could be re-allocated to better meet the needs of the population. In this example, rather than an uncontrolled closure, the area would be better served by distributing resources between other right-sized facilities in strategic locations. The Blueprint would allow us to:
- Shift one facility to a rural emergency hospital, which protects vital emergency services while cutting overhead expenses.
- Resources could then be reinvested in an ambulatory health park in an underserved part of the region, offering a freestanding ED plus primary care, outpatient surgery, and some behavioral health services. Given the right location, this AHP should be sustainable for its operator.
- Without the drag of a half-empty small rural hospital, the shifting patient volume would allow one of the remaining facilities to convert to a regional referral center, drastically cutting the drive time for more complex, specialized care.
With all of these improvements in accessibility and service variety, Region Z would see its score increase to 71.0. This scenario not only offers better health outcomes, but it is also more financially sustainable under market conditions.